
The Contextual Kits for T2CT have been designed to enhance thermal place preference studies...

The Contextual Kits for T2CT have been designed to enhance thermal place preference studies...

An easy way to objectively quantify the muscular strength of mice and rats, and to assess the...
The BIOSEB Spontaneous Activity Wheel offers an effective solution for quantifying rodent...

The BIOSEB Spontaneous Activity Wheel is an easy way to quantify rodent voluntary activity in...

The uncomplicated way to monitor rodent activity over several days from their home cage...

These small animal treadmills are used for forced exercise training and accurate testing of...

For testing animal's thermal sensitivity to pain resulting from exposure to heat or cold: the...

An operator independent test to study pain thresholds in rodents (mouse and rat) by assessing...

New and improved! The operator-independent Thermal Gradient Test used to show favorite...

The Contextual Kits for T2CT have been designed to enhance thermal place preference studies...

The advanced version of our Dynamic Weight Bearing Test for rodents (rats and mice) allows for...

An easy and non pain-inducing solution for assessing the level of discomfort (incapacitance) in...

A unique device that provides automated measurement of weight bearing and force distribution...
![Dynamic Weight Bearing 2.0 – Postural Module [Add-on]](https://bioseb.com/733-home_default/dynamic-weight-bearing-20-add-on-postural-module.jpg)
Expand Your Analysis with Advanced Postural and Locomotor Calculations BIOSEB’s renowned...

A quick solution to determine the mechanical sensitivity threshold in rodents (mice and rats)....
As an electronic version of the classical Von Frey Filaments esthesiometer (or aesthesiometer),...

New ROBUST and modular cages to gently hold rodents (rats or mice) during nociceptive and...

An economical and versatile solution for when flexible quantitative sensory testing (QST) is...

Dedicated to small animals, like mice and rats, Smalgo is a pressure-based analgesimeter...

Bioseb's version 5 of the Tail Suspension Test system, based on both strain sensors and video...
NEW ! A complete (hardware + software), dedicated and automated solution for the Elevated Plus...

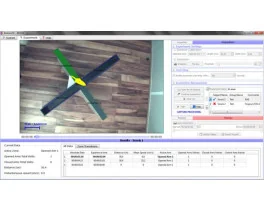
A unique setup for the automation of the Open Field test for rats and mice : 3D-camera based...

Open-field test - ARENA ONLY - used to evaluate of animal's basal activity and its evolution for...

The new Forced Swimming Test system from Bioseb uses a dual approach: Combining a double input...

A brand new innovative setup for the automation of the Novel Object Recognition Test : 3D-camera...

Open-field test - ARENA ONLY - used to evaluate of animal's basal activity and its evolution for...

An entirely modular experimental enclosure designed to conduct operant conditioning procedures...

A standard experimental chamber for automated or manual assessment of conditioned place...

Real-Time Physiological Monitoring for Small Animals – Wireless & Non-Invasive The Bioseb...

The ETH-401 is a bridge amplifier for various transducers that provides four channels of...

The IX-118 is a fast 100 Khz, high-resolution data acquisition system suitable for most data...

The ETH-256 is a 2 channels high performance, general-purpose life science research amplifier,...

Discover BIO-FOODIS, the next generation solution for understanding animal feeding behavior with...

The OXYLET system - Physiocage is a modular system allowing the integration of respiratory...

Innovative and appropriate equipment for measuring food/liquid consumption and correlated motor...
An economical, high performance Oxygen and Carbon Dioxide Analyzer with sampling rates fast...
10/18/2024 News & Events

Opioids have revolutionized pain management, but they carry significant side effects that can result in respiratory failure and even death. The opioid crisis has significantly impacted the United States since the 1990s. Addiction to these painkillers has spread like an epidemic.
Despite a fall compared to 2018 (84,181 deaths), the number remains alarming. These opioids, developed to relieve severe pain, have thus become addictive drugs, causing a public health problem with considerable economic cost. Against this backdrop, preclinical studies are central to respond to the opioid crisis. They help to better understand and manage the side effects of painkillers and to develop alternative treatments. Here is an overview of current research examples and the tools available.
The US National Institutes of Health (NIH) HEAL (Helping to End Addiction Long-term initiative) plays a key role in the development of non-addictive treatments for pain. In 2023, it supported more than 314 clinical trials and filed 41 applications with the FDA to test new drugs or devices, doubling its submissions from the previous year. Of these projects, more than a hundred were for back pain and more than 200 were for drugs for opioid use disorders (NIH HEAL Initiative). In this initiative, the focus is on safer and more effective treatments for pain and addiction, in particular through public-private partnerships to test promising compounds that have been abandoned.
Although opioid analgesics are effective in relieving pain, they are associated with a wide range of side effects, from mild to severe. The most common include drowsiness, constipation and nausea, but more serious complications, such as respiratory depression, can be life-threatening. Opioids can also induce euphoria, which increases the risk of overuse and dependence. In the United States, they are responsible for the vast majority of drug overdoses. Fentanyl, for example, a synthetic opioid fifty times more powerful than heroin, was detected in 81% of overdose cases in New York in 2022
To prevent these serious consequences, it is essential to identify the side effects of opioids at an early stage of the drug development process. The animal models used in preclinical studies play an essential role in this effort. For example, rodents have been used to explore how chronic exposure to opioids can lead to changes in brain chemistry underlying addiction. An important area of preclinical research has focused on understanding opioid-induced respiratory depression, a major cause of overdose death. A study by Montandon and Horner (2014) used rodent models to explore how opioids affect respiratory circuits at a central level. The work demonstrated that chronic exposure to morphine in rodents resulted in significant respiratory depression mediated by brainstem respiratory centres.
Animal models are also essential for studying both the addictive properties of opioids and their effects on prenatal development. They provide a controlled environment in which to study the direct effects of opioid exposure in utero, for example. Indeed, neonatal opioid withdrawal syndrome (NOWS) is difficult to study in humans due to the complexity of maternal drug use and environmental factors. A review by Ferrante and Blendy (2020) highlighted studies that also reveal how these models have improved understanding of prenatal opioid exposure, influencing early diagnosis and treatment strategies.
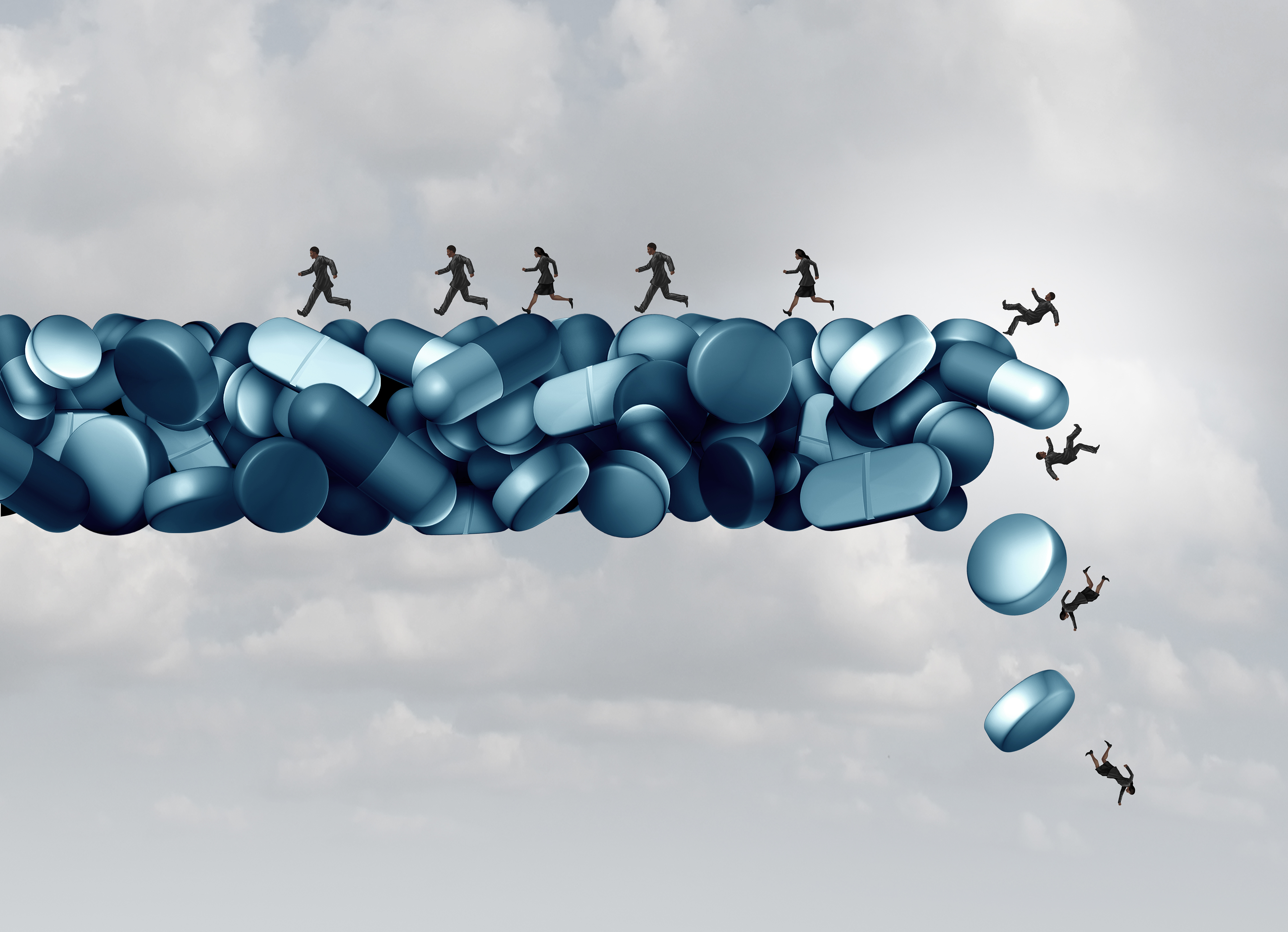
The consequences are devastating, with an explosion in the number of overdoses. According to the Centers for Disease Control and Prevention (CDC), over 81,083 people died from opioid overdoses in the U.S. by 2023.
The development of new compounds with a better risk-benefit ratio is among the solutions to avoid opioid dependence, as well as their unsatisfactory safety profile.
One such approach involves the design of biased μ-opioid receptor agonists, which aim to relieve pain without the full range of side effects associated with traditional opioids. For example, work by DeWire et al. (2013) showed that TRV130, a biased agonist, produced potent analgesia in rodent models with reduced respiratory depression and gastrointestinal side effects compared to morphine.
Many other strategies have been developed, including the use of activators of specific μ splice variants (Majumdar et al., 2011), a pH-dependent μ agonist (Spahn et al., 2017) or a dual nociceptin/μ agonist (Ding et al., 2018). A scientific team has developed an original design that is independent of the μ-opioid receptor. The researchers showed that targeting TREK1, the potassium channel involved in the antinociceptive activity of morphine, but not in its adverse effects, completely dissociates the antinociceptive and adverse effects of morphine.
Among the devices used, tests to evaluate motor coordination were also performed, such as the Rotarod, which measures the time it takes for an animal to fall from a rotating rod whose speed gradually increases. The mechanical pain thresholds were assessed using Von Fey filaments. The results of the study show that selective pharmacological activation of TREK1 is a promising and safe strategy for relieving pain.
The search for non-opioid alternatives is also a major focus of preclinical studies. Given the addictive potential of opioids, there is an urgent need to develop effective pain treatments with a better safety profile. One promising approach to pain associated with certain pathologies, such as osteoarthritis, which is sometimes relieved by opioids, is the use of local anaesthetics (LA). University of Connecticut researchers (Kishnan et al., 2023), used a rodent model to compare the efficacy of periarticular versus intra-articular administration of LA in the management of osteoarthritis pain. They used the Electronic Von Frey device and a pressure sensor system from Bioseb to measure mechanical allodynia. The results showed that periarticular injections provided significantly longer-lasting pain relief, with a prolonged analgesic effect for up to 17 days, superior to traditional intra-articular injection, suggesting that LA could be a viable alternative to opioids for certain types of pain.
Neuropathic pain, caused by injury or dysfunction of the somatosensory system, is very difficult to treat without opioids. A study by Sun et al. (2022) investigated the PTPRD receptor, linked to addiction pathways, which could play a role in neuropathic pain. The results show that a small molecule (7-butoxy illudalic acid analogue: 7-BIA) reduces neuropathic pain in rats while activating a pathway involved in the immune response. The discovery of the possibility of using this compound could be a new therapeutic option for managing neuropathic pain without the risk of addiction, made possible by the animal model: pain sensitivity (temperature and thermal latency of paw withdrawal) assessed using a Cold Hot Plate test (Bioseb).
A French team (Girard et al., 2008) explored the antinociceptive synergy between nefopam, a centrally acting non-opioid that inhibits monoamines reuptake, and ketoprofen, a non-steroidal anti-inflammatory drug. The scientists used Bioseb's Smalgo device to accurately measure pain responses, demonstrating the increased efficacy of this combination in reducing pain while minimising side effects.
Non-pharmacological approaches include various therapies that do not involve medication, focusing instead on holistic and often multimodal strategies. These include physical therapy, cognitive-behavioral therapy (CBT), acupuncture, chiropractic care, mindfulness meditation, and other integrative health techniques. Evidence suggests that these methods can effectively manage various types of pain, including chronic pain, back pain, arthritis, and neuropathic pain. These alternatives are supported by the National Institutes of Health (NIH) and other leading health organizations to reduce the risks associated with opioid use while effectively managing pain.
The opioid crisis in the United States underscores the critical importance of preclinical studies in addressing the side effects of painkillers and developing safer, more effective treatments. Researchers have a key role to play in ensuring patient safety and preventing the misuse of opioids. As we continue to face this public health challenge, it is essential to strengthen research and monitoring protocols. Bioseb is committed to supporting preclinical research and promoting rigorous practices in the development of new medicines. By advancing our understanding of opioid effects and exploring alternative therapies, we can move toward a future where pain is managed effectively and responsibly.

1. Montandon G, Horner R. CrossTalk proposal: The preBotzinger complex is essential for the respiratory depression following systemic administration of opioid analgesics. J Physiol. 2014 Mar 15;592(6):1159-62.
2. Ferrante JR, Blendy JA. Advances in animal models of prenatal opioid exposure. Trends Neurosci. 2024 May;47(5):367-82.
3. DeWire SM, Yamashita DS, Rominger DH, Liu G, Cowan CL, Graczyk TM, Chen XT, Pitis PM, Gotchev D, Yuan C, Koblish M, Lark MW, Violin JD. A G protein-biased ligand at the μ-opioid receptor is potently analgesic with reduced gastrointestinal and respiratory dysfunction compared with morphine. J Pharmacol Exp Ther. 2013 Mar;344(3):708-17.
4. Majumdar S, Grinnell S, Le Rouzic V, Burgman M, Polikar L, Ansonoff M, Pintar J, Pan YX, Pasternak GW. Truncated G protein-coupled mu opioid receptor MOR-1 splice variants are targets for highly potent opioid analgesics lacking side effects. Proc Natl Acad Sci U S A. 2011 Dec 6;108(49):19778-83.
5. Spahn V, Del Vecchio G, Labuz D, Rodriguez-Gaztelumendi A, Massaly N, Temp J, Durmaz V, Sabri P, Reidelbach M, Machelska H, Weber M, Stein C. A nontoxic pain killer designed by modeling of pathological receptor conformations. Science. 2017 Mar 3;355(6328):966-9. Erratum in: Science. 2017 Jun 9;356(6342).
6. Ding H, Kiguchi N, Yasuda D, Daga PR, Polgar WE, Lu JJ, Czoty PW, Kishioka S, Zaveri NT, Ko MC. A bifunctional nociceptin and mu opioid receptor agonist is analgesic without opioid side effects in nonhuman primates. Sci Transl Med. 2018 Aug 29;10(456).
7. Busserolles J, Ben Soussia I, Pouchol L, Marie N, Meleine M, Devilliers M, Judon C, Schopp J, Clémenceau L, Poupon L, Chapuy E, Richard S, Noble F, Lesage F, Ducki S, Eschalier A, Lolignier S. TREK1 channel activation as a new analgesic strategy devoid of opioid adverse effects. Br J Pharmacol. 2020 Oct;177(20):4782-95. Erratum in: Br J Pharmacol. 2020 Nov;177(22):5246.
8. Kishnan D, Walker J, Nair L. Minimally invasive periarticular injections of local anesthetic provides prolonged analgesia in a rodent osteoarthritis model. J Pain. 2023 Apr;24(4 Suppl):25.
9. Sun C, Wu G, Zhang Z, Cao R, Cui S. Protein Tyrosine Phosphatase Receptor Type D regulates neuropathic pain after nerve injury via the STING-IFN-I pathway. Front Mol Neurosci. 2022 Apr 14;15:859166.
10. Girard P, Verniers D, Coppé MC, Pansart Y, Gillardin JM. Nefopam and ketoprofen synergy in rodent models of antinociception. Eur J Pharmacol. 2008 Apr 28;584(2-3):263-71.
check_circle
check_circle